When Katherine Imborek, MD, has a patient with an unfamiliar rash or skin lesion, she often takes a picture with an iPad, securely uploads it to the patient’s electronic medical record (EMR), and sends it to a dermatologist. The dermatologist looks at the image, reviews the patient’s chart, and might suggest that Imborek prescribe a particular medication or treatment rather than referring the patient to a dermatologist.
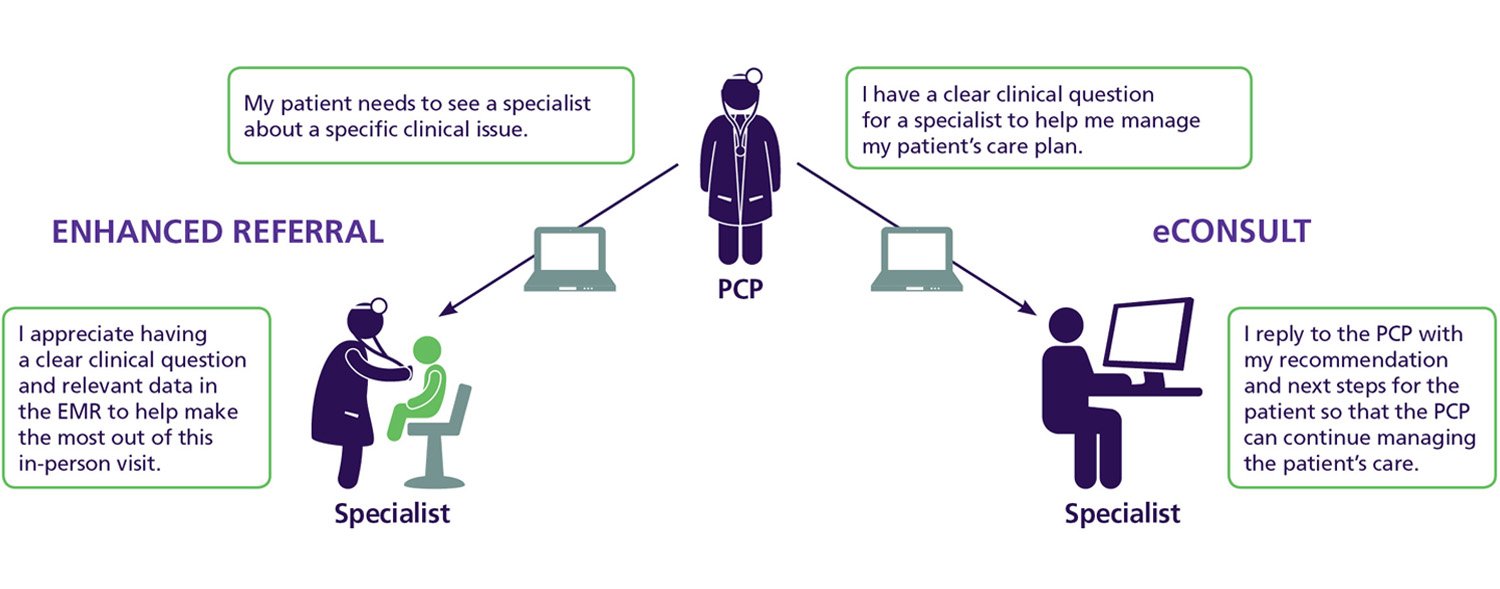
This interaction, known as an eConsult, simplifies the process of seeking input from specialists, allowing primary care physicians (PCPs) to ask specialists specific clinical questions when they aren’t quite sure how to treat a problem that might not require a face-to-face visit with a specialist. Starting in 2014, the AAMC, with a grant from the Center for Medicare and Medicaid Innovation, has worked with five academic health systems to pilot the eConsult platform, known as Project CORE (Coordinating Optimal Referral Experiences). Since then, an additional seven health systems have implemented the model, and the AAMC anticipates adding a third cohort this year.
Project CORE is a “no brainer” if payers are on board, said Imborek, director of off-site primary care at University of Iowa Health Care. “This aligns with strategic plans at many institutions in terms of patient satisfaction, improving access, and improving care.”
Improved communication with specialists
By enhancing communication and coordination between PCPs and specialists, Project CORE has reduced demand for specialist visits for more routine problems, freeing up time for specialists to see patients with more serious problems. In the project’s first 18 months, the more than 8,000 eConsults at the five pilot sites avoided an estimated 3,600 specialist referrals, said Scott Shipman, MD, MPH, AAMC director of primary care affairs and workforce analysis and the project’s principal investigator.
A 2012 Archives of Internal Medicine article reported that the number of specialist referrals has more than doubled in the United States since 1999. And the number of new specialists is not keeping pace with demand, according to an AAMC-commissioned study released in March 2017 that projected a shortage of between 33,500 and 61,800 nonprimary care specialists by 2030.
“As we face increasing demand alongside the shift to risk-based reimbursement models, a distinct advantage of this model is that it improves access, promotes high-quality care at lower costs, and increases satisfaction for providers and patients,” Shipman said.
“Specialists provide education on clinical topics PCPs may not be as comfortable dealing with on a day-to-day basis. This, in turn, allows patients to remain in their primary care medical home and avoid an unnecessary specialist visit.”
Michelle L’Heureux, MD
Dartmouth-Hitchcock
In Iowa, Imborek said Project CORE has helped PCPs think about which patients “can be managed and, in some cases, even better managed by their PCP with whom they’ve had longstanding relationships and whom they trust.” By keeping those patients with their primary doctor, specialists have more time to see patients with more serious problems. “It really helps us hone in on assuring only those patients with complex medical issues are the ones who see the specialist face-to-face,” Imborek said.
Communication: A path to success
Nathaniel Gleason, MD, an internist at the University of California, San Francisco, initially developed this eConsult model to address the needs of an academic health system. When he first proposed the idea to specialists, he was surprised to learn that they didn’t think it would work. In the days of paper charts, referrals didn’t always include enough information for specialists to give an opinion without also taking the time to comb through the patient’s chart. As EMRs became more common, referrals didn’t necessarily become more detailed. “Specialists were very frustrated by the limited information. When we asked them if they could answer some of our questions electronically, they were picturing that terribly limited referral and said no,” Gleason said.
He stepped back and developed an electronic template that would give specialists the information they needed to provide a recommendation without having to look through the patient’s chart. He also tried to better understand what treatments or tests primary care providers should suggest before sending a patient to a specialist. For example, he asked cardiologists to meet with PCPs to explain treatment protocols for common issues. “We wanted them to talk about coronary artery disease, heart failure, and atrial fibrillation—conditions we commonly manage in primary care, but sometimes refer to cardiology. We tried to set the expectations in terms of what [the specialist] wants us to do before referring.”
That dialogue between specialists and PCPs has been key to Project CORE’s success. At Dartmouth-Hitchcock, one of the five initial sites, the program has improved access to specialists, but PCPs have been especially satisfied with the opportunity to learn from specialists. “Specialists provide education on clinical topics PCPs may not be as comfortable dealing with on a day-to-day basis. This, in turn, allows patients to remain in their primary care medical home and avoid an unnecessary specialist visit,” said Michelle L’Heureux, MD, a general internist at Dartmouth-Hitchcock and the site’s primary care lead for Project CORE.
Project CORE has become the standard of care at Dartmouth-Hitchcock, which operates more than 20 clinics throughout New Hampshire. Initially there were challenges in getting PCPs to use eConsults, particularly physicians at sites that are far away from the main teaching hospital. Some specialists were also hesitant about the new model. PCPs and specialists worked collaboratively to design and modify the eConsult templates, which contributed to the project’s success. “I think one of the main contributing factors that made this model successful at Dartmouth-Hitchcock was getting as many stakeholders [as possible] involved in the process early on, so that everyone had a chance to give their input,” L’Heureux said.
The next challenge is demonstrating to payers that they should reimburse providers for eConsults. “In the Project CORE model, specialists are providing care when they make recommendations to primary care providers. Such care is not supported in traditional payment models. But by reducing unnecessary specialist visits and tests, this model can reduce overall costs, to the benefit of patients and payers alike,” Shipman said.
