Restricting calories, vomiting after meals, occasionally bingeing and purging — it all made Meg Haston, then a college freshman, feel somewhat in control of her anxiety and depression. She knew she had an eating disorder, but it took an ultimatum from a therapist to get to in-patient therapy. She felt scared but also relieved. Then after treatment, she found out that her insurance provider refused to cover her 45-day stay, leaving her with a bill for $30,000. The reason why hit Haston, a truly sick person obsessed with being thin, where it hurt: They said her weight wasn’t low enough to justify reimbursement.
“There is nothing more invalidating than being told you’re not ill enough to merit care,” says Haston, now 34. “One of the scripts I played in my head was, ’I’m not thin enough to go to treatment, not sick enough.’ The insurance company confirmed this.” Had she been “thin enough,” she might have been near death.
Haston’s story illustrates a sad reality faced by eating-disorder sufferers: It’s really hard for them to get the help they need. Even some experts don’t believe they need it unless they’re shockingly thin. Too many health-care professionals aren’t properly trained to spot an ED. And mental illnesses are often trivialized, especially those that disproportionately affect women. “People are easily dismissed,” says Johanna S. Kandel, the founder and executive director of the Alliance for Eating Disorders Awareness. “There’s so much shame and stigma.”
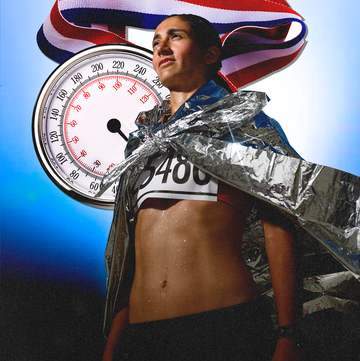
Why is something so common treated with so much disdain? One in 11 Americans will develop an eating disorder, per the National Eating Disorders Association. And they’re not all starving themselves.
Eating disorders aren’t necessarily about weight or even food. They’re bio-psychosocial disorders, with roots in genetics, emotions, behaviors, and social, environmental, or cultural factors. EDs often go hand in hand with other mental illnesses, like depression, anxiety, and OCD. Pressures to have a perfect body aren’t the sole trigger — abuse, trauma, and appearance-related teasing also raise risk. As does family history: Up to 80 percent of your risk for developing one is due to genetic factors.
With any other disease that is innate or, at the least, involuntary, wouldn’t we try to make life easier, not harder?
“The majority of people with eating disorders may not be emaciated. Most are normal or overweight,” Kandel says. In fact, binge-eating disorder — whose sufferers don’t generally lose weight — is more common than anorexia nervosa (self-induced starvation) and bulimia nervosa (bingeing and purging) combined. “It’s not how people think of eating disorders. They don’t think non-thin sufferers need professional help.”
Insurance policies seem to reflect these misperceptions. Treatment may not be covered if you aren’t deathly ill (so sick that you’ve had a cardiac event, for example). Creepier still, you could be denied coverage if you aren’t dangerously thin, often designated as less than 85 percent of healthy weight for your height.
But even if a woman is emaciated, simply focusing on the number on the scale misses the point. In dire cases, the first step of treatment — before a psychological regimen can start — is to get the patient to a healthy size so she can survive. Cutting off coverage before counseling begins means she has gained weight (likely a scary prospect for her) but has made little, if any, progress toward truly healing. Physical diseases typically have clear benchmarks that indicate a patient is well, but mental illnesses don’t have black-and-white distinctions. Just because a person weighs a certain amount doesn’t mean she’s better, experts say.
“If you had cancer, your doctor would treat you until every speck of cancer is gone,” says Lisa S. Kantor, partner at Kantor & Kantor, a law firm in Northridge, California, that focuses on claims against insurers. “With eating disorders, insurance companies have an attitude that they can get you 75 percent there, then send you home. If you don’t do well, you go back. Of course, you won’t do well if you haven’t eradicated as many symptoms as possible.”
Cosmopolitan contacted several health-insurance companies for comment and was directed to America’s Health Insurance Plans, an association that represents insurance companies. “Health plans coordinate with providers, specialists, and families to develop care plans that address the individual needs and circumstances of each patient and are aligned with medical evidence around safety and effectiveness,” Clare Krusing, a spokeswoman for the association, replied via email. “If there is a lack of agreement, clinicians and patients have the right to appeal — a patient right that our industry has long supported.” Krusing’s statement didn’t specifically address the 85 percent practice.
There’s a dark side to that appeals process. “People die from eating disorders. A lot of coverage denials don’t get to litigation,” says Alicia Paulino-Grisham, an attorney in Florida who represents eating-disorder and cancer patients against insurance companies. “They’re either too sick to challenge it or there’s a good chance they’ll pass away beforehand.”
By the time Michelle Z., 22, of Deerfield, Illinois, got to college, she’d been dealing with undiagnosed anorexia for years, skipping meals and obsessing over her size. She confided in a friend, who encouraged her to seek treatment. She made an appointment with a doctor at the university health center. According to the physician’s online listing, Michelle says, she was an eating-disorder specialist.
Michelle told the doctor about her issues: restricting food, overexercising, and struggling emotionally. “She responded, ‘You don’t look like you have an eating disorder,’ because I wasn’t underweight,” Michelle recalls. “I remember thinking that must mean there’s nothing wrong with my behavior. Her nonchalance disempowered me and gave power to the disorder.”
Even when a patient does look like the stereotype of a rail-thin anorexic, society’s glorification of thinness can get in the way of treatment, notes Bernice Pescosolido, PhD, director of the Indiana Consortium for Mental Health Services Research. “Given how much we admire thin people, it’s hard to comprehend when someone is in trouble,” she says. Haston describes going to the doctor for a physical at a point when she was at her lowest weight. As she was being weighed, the nurse whispered, “How do you stay so skinny? I wish I knew your secret.” Says Haston, “My secret was that I was ill.”
Many med schools don’t provide doctors-to-be with the proper training in recognizing and treating eating disorders, adds Edward P. Tyson, MD, a physician in Austin who specializes in EDs. “You have to seek out practitioners who themselves have sought out specific training. Medical schools spend very little time on the subject ... and usually, they get it wrong,” he says. But specialists and treatment centers are in rare supply. Eight states have just one ED treatment center. Twelve have none at all. Such specialized care is key, says Claire Mysko, CEO of the National Eating Disorders Association. “Hospitals can treat the physical issues and some of the psychiatric ones, but an eating disorder is a complex illness. Patients are best served by seeing doctors, psychologists, and nutritional counselors with clinical experience in this field.”
The Association of American Medical Colleges, which represents all accredited U.S. medical schools and nearly 400 teaching hospitals, counters that eating-disorder info is disseminated in most med schools. “Of those institutions that participate in the AAMC’s curriculum inventory, 74 percent reported covering eating disorders,” says John Prescott, MD, AAMC’s chief academic officer.
Still, Dr. Tyson believes that some doctors just aren’t comfortable with eating disorders — and sexism may play a role. While men do get eating disorders, it’s still widely thought of as a women’s issue. “If men had 90 percent of the eating disorders,” Dr. Tyson says, “I suspect we would have a lot more research, advocacy, and awareness.”
Meg Haston and Michelle eventually got treatment — in Michelle’s case, largely thanks to friends. That makes her lucky in a way — some sufferers experience outright repudiation. Greta W., now 24, from Boston, claims she was fired from her on-campus job and asked to leave school because of her ED. She confided in a friend about having an ED and suicidal thoughts, and the friend went to authorities, presumably to get help. Her school forcibly removed her from campus in an ambulance, then put her under around-the-clock watch once she was allowed to return. It all made Greta feel “like a criminal ... for a crime I didn’t commit.”
Getting kicked out of school sounds extreme, but it happens, says Paulino-Grisham: “Colleges don’t want students to die at their institution.” Most schools don’t even have a policy for dealing with ED, says Jessica Setnick, RD, author of the forthcoming book Managing Eating Disorders on Campus. “It should be a buzzword, like hazing or binge drinking,” she says. “Every college should have a task force, with this many counselors and dietitians for this many students.”
Employers might not handle things any better. Even well-intentioned wellness programs may be triggering, says Mysko: “They often put an emphasis on obesity and weight loss. Instead, programs should address health in a holistic way.” Including eating disorders in employee-assistance programs (for example, offering screening tools) is one strategy for reducing stigma and delays in treatment. As it stands, Kandel says, “an ED sufferer might not say anything for fear of ramifications.”
If someone confides in you, acknowledge how difficult it must be to open up, suggests Kandel, but let her know that her health is more important than any job. Direct her to her company’s EAP or myNEDA.org, and offer to go with her to speak with a supervisor or HR rep.
Eating disorders are intense and scary. Anorexia alone kills more people than any other mental illness does. But while the stakes are high, with the right treatment, they are curable. Says Kandel, “We need greater awareness of what eating disorders look like, what causes them, and that people can recover.” That is, if we help them.
This article was originally published as "HELP" in the November 2016 issue of Cosmopolitan. Click here to subscribe to the digital edition.